Mental health crisis amongst Yazidis in Iraq
"I am always thinking about the memories from the genocide, those who died, those who emigrated"
The Yazidi community in Sinjar district, north western Iraq, is grappling with a severe and debilitating mental health crisis, including a high number of suicides and suicide attempts.
Between April and August 2019, 24 patients who were brought to the Emergency Room (ER) of Sinuni’s hospital had attempted suicide- six of whom died before arrival at the hospital or were unable to be saved. Of the 24, 46% were under 18 – the youngest a 13-year-old girl who hung herself and arrived dead at the ER. 54% were women or girls, four died of self-immolation. Others attempted suicide by self-injury to their wrists, drinking poison, overdosing on medication or with firearms.
In the small town of Sinuni, which became the centre of gravity for the long-persecuted Iraqi Yazidi minority that remained in the area, MSF started offering mental health consultations in December 2018. Since then, 286 people have been enrolled in the programme, of which 200 are still under treatment today. The most common diagnosis is depression (40%), followed by conversion disorder[1] (18%) and then anxiety (17%). Some psychiatric and personality disorders, including post-traumatic stress disorder (3%), have also been diagnosed. Even though MSF Mental Health services in the area were scaled up in recent months, they are now overwhelmed and with a waiting list.
On World Mental Health Day, MSF calls for an increase in both international and national investment in mental health care, not only in Sinjar district but across an Iraq still reeling from years of brutal wars and economic instability.

In their own words
Amina Ismail Elias, 20, poses in her house on Mount Sinjar on September 3rd, 2019.
I am very very depressed. Medication makes me sleepy to I stopped taking the pills. I didn’t go to school at all, don’t know how to read or write. I don’t do anything, not even house chores.
About 20 days ago, I tried to kill myself by cutting my wrists. When we were IDPs in Kurdistan I tried to set myself on fired and to get killed by a car. Why? I don’t really know.
I am depressed. It started six years ago when one of my uncles was killed. Sometimes I faint and remain unconscious. I am always falling. I have pain in my skull from falling so much. Sometimes, I sit like that, and stay like that for hours.
In 2014, we had to flee, but I don’t remember anything from that time. I blocked all the memories. Whenever I fight with someone, especially my father, I think about suicide. I just want to be like before, to be normal. I would give half of my lifetime to be normal.
©Emilienne Malfatto
©Emilienne Malfatto
©Emilienne Malfatto
©Emilienne Malfatto
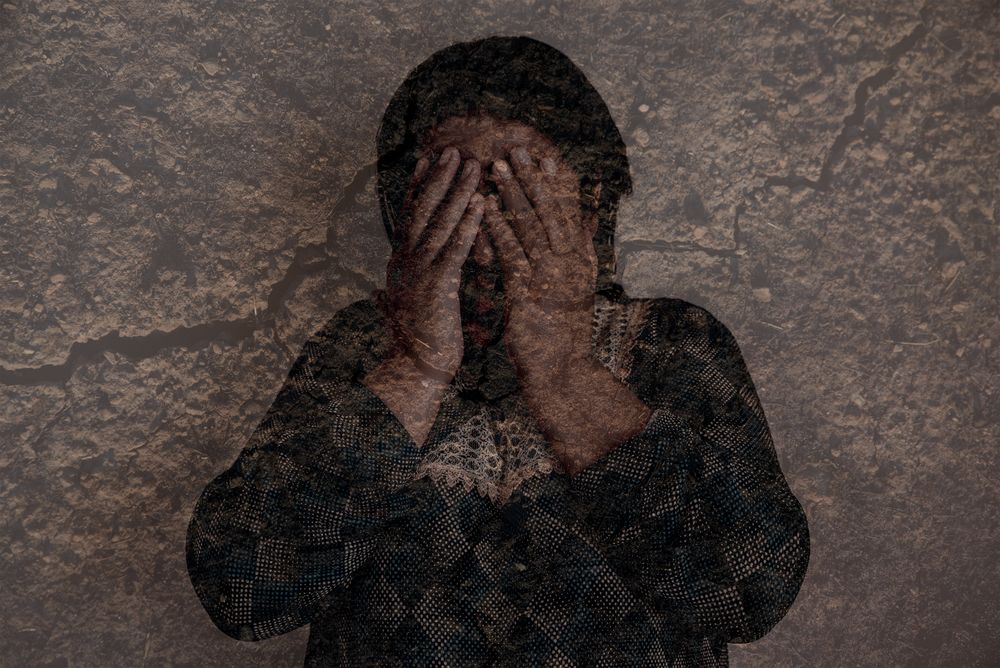
A Yazidi woman aged 60 poses in her house in Sinuni on September 2nd, 2019.
We are from Khanasor village but we’ve been living in Sinuni since March 2019, when we came back from the IDP camps.
After the 2014 genocide, I started to have mental health problems. I feel nervous, scared, uncomfortable and angry. I have a constant headache. I have pain in my eyes because I cry a lot.
I am always thinking about the memories from the genocide, those who died, those who emigrated. Some of my sons live abroad now, and it’s difficult to be apart.

“Our first mental health survey in 2018 in Sinuni revealed that 100%** of the families we spoke with had at least one member who suffered either moderately or severely from mental illness,” said Dr Marc Forget, MSF’s Head of Mission in Iraq. The magnitude of the needs was confirmed by authorities. “When we met with the medical director of the Hospital in Sinjar, the heavily destructed town on the other side of the Sinjar mountain, he told us that everyone needs mental health support in the district, including him. It matched what we realized soon into the beginning of our activities: that we were dealing with a major mental health crisis, and also that there was something specific to it, directly linked with the collective trauma Yazidis endured recently.”
In August 2014, the Islamic State group attacked the Yazidi religious minority living in the region. What followed has been the scene of a tragedy: a sustained campaign of killings, rape, abductions and enslavement, followed by a mass migration, mainly to camps in the adjacent Kurdish region. The UN has acknowledged IS’s atrocities in Sinjar region as genocide. Whilst the Sinjar area was retaken from the IS group more than four years ago, the return of those who fled the area has been slow. Still today many Yazidi families prefer to stay in Iraqi Kurdistan rather than return to their homes. This is not only because many home and villages lay decimated, are littered with landmines and lack basic services like water or electricity but also because of the trauma many Yazidi now associate with their ancestral homelands.
[1] 52 people participated to this survey conducted in September 2018.

In their own words
Hassan Khudeda Qasim, 51, poses in his home on Sinjar mountain on September 3rd, 2019.
I have been living on the mountain all my life. My family used to be rich, but then three of my brothers got in a bad situation and we became poor 17 years ago. That is when my problems started.
I have psychosis. I have been taking medication since 2002. I am angry and upset all the time. I am overthinking all the time. I have insomnia and headache. If I don’t take my medication, I become scared and angry and sometimes violent with my children.
When that happens, my wife and children are afraid of being around me. I like to be alone. I have suicidal thoughts. Since 2014, my problems have worsened. We were on the mountain then escaped to Syria. We were IDPs in Kurdistan for two years then came back to Sinjar. I have six children and no job. We are very poor.
©Emilienne Malfatto
©Emilienne Malfatto
©Emilienne Malfatto
©Emilienne Malfatto
In their own words
Halo Khalaf, 66, poses in her house in Sinuni on September 2nd, 2019.
We are originally from the South of Mount Sinjar. I have no children. My husband died before the genocide. Before 2014, I was living with my only brother Khader and his family. Khader was kidnapped by ISIS and never returned.
We were actually kidnapped together, but I could escape after 20 days in captivity. I keep waiting for Khader. I wait for all the abducted ones to come back. So many people in my family have been kidnapped. Almost all my brother’s family has been kidnapped.
Some came back, some didn’t. One of my nephews is currently with ISIS in Al-Hol camp in Syria. He has been brainwashed, he changed his name and doesn’t want to come back. I just with the kidnapped ones would come back. My dream is to save them. I pray everyday for God to bring back my brother.
Before the genocide, I didn’t have any psychological problems, or health problems. Now I must take a lot of medication. I have mental health problems, kidney problems, high blood pressure, colon problems… I always feel like ISIS is coming.
When I sleep, I wake up with a start. I cannot see clearly because I cry a lot. I feel pain in my whole body. I am not happy.

“Everyone here has lost at least one family member or friend and all over Sinjar region there is overwhelming sense of hopelessness and loss,” says Dr Kate Goulding, who works in MSF’s emergency room in Sinuni. “It is universal to be sad when your husband dies, when your child is sick, when you break up with your partner or when you are forced to be away from your family. But the extent of loss in this community is incomprehensible and compounded by the trauma of extreme violence, humiliation, mass displacement, poverty and neglect. As everyone will tell you here, the genocide perpetrated by IS wasn’t the first genocide the Yazidi have survived, it was the 74th,”
Dr. Goulding supported MSF’s Yazidi staff to care for psychiatric patients for two months this year whilst MSF was unable to find a psychiatrist in Iraq. This is indicative of a larger issue in the country, where there is inadequate number of trained psychiatrists, psychologists and mental health counsellors to meet the immense mental health needs surfacing after years of brutal violence.
“Despite the urgency of the situation in Sinjar, we are unable to find qualified psychiatrists and psychologists in Iraq to work with us. So as MSF we are forced to bring in international staff for support, which is not ideal, and also not sustainable in the long term” says Dr Marc Forget, MSF’s Head of Mission in Iraq. “The Iraqi mental health system definitely needs more money and more medication, but the biggest need is for more qualified staff, and for them to be assigned to areas of greater shortages, especially in rural and conflict affected areas of this country.”

MSF in Sinuni
An MSF team began supporting the Sinuni General Hospital with emergency and maternity services in December 2018 and quickly realised that mental health was a huge unmet need in the area. Since then, the team has increased the mental health care activities to cover psychiatric and psychological health care activities in Sinuni hospital as well as group sessions and mobile mental health clinics for the displaced-on Sinjar mountain.
Beyond the mental health clinic, since the beginning of 2019 MSF staff have conducted 9770 consultations in the emergency room, 6390 for further treatment in the in-patient wards and assisted 475 women to bring their babies safely into the world.
*Conversion disorder is a mental condition where a patient experiences blindness, paralysis, or other nervous system symptoms that cannot be explained by medical evaluations.
**52 people participated to this survey conducted in September 2018.






